“iridotomy” is the name of a laser procedure preformed for eyes with narrow angles, eyes that are at risk for “angle-closure glaucoma”
.Alternative names for this common procedure include: laser peripheral iridotomy, iridectomy, and in short: LPI or PI.
One characteristic of most people who need this treatment is the fact that they are more often than not, completely healthy, with no prior eye problems, when suddenly, their ophthalmologist decides, quite unexpectedly, that they need laser treatment. Indeed, this is not pleasant news, and some of you will certainly sit down in front of your computers and surf the web in an attempt to find out why a seemingly healthy individual suddenly needs a laser procedure for their eyes. This page will provide you with explanations and additional information about this condition and about possible treatment options.
As a rule, patients who require laser iridotomy treatment can be divided into two groups: the few who have experienced (or who are now experiencing) an acute attack of closed-angle glaucoma, as opposed to those who are in danger of developing such an attack in the future. We will begin with answering the following question: what is an acute attack of closed-angle glaucoma?
Well, it refers to an acute condition in which the intra-ocular pressure rises suddenly to extremely high values. Such an eye will suffer from very intense pain, redness, and blurred vision. The pain is so severe that in most instances the person will decide to head to the emergency room, with complaints of extreme pain in the eye, occasionally accompanied by severe headaches. This pain is often associated with nausea and vomiting, and it is common for the pain and nausea not to be attributed (by the patient and at times by the doctor as well) to an eye problem, because it is so intense. These patients are classified as seriously ill, due both to the pain as well as the potential serious damage that can occur to the eye by such a significant increase in pressure. The treatment needed to terminate such an attack often starts with medications aimed at reduction of pressure, given as drops and pills.
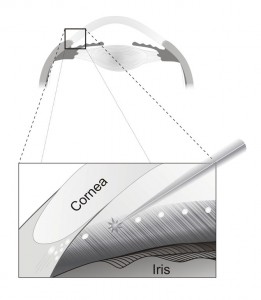
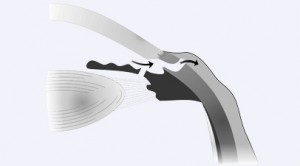
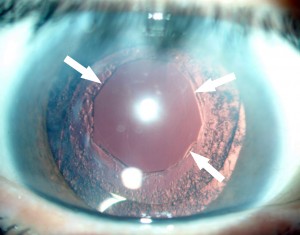
After a certain decrease in intraocular pressure (and pain) it is possible to begin a more focused solution to this acute problem. This next step in treatment includes creating a small internal aperture (a small internal hole) within the eye which serves to equalize pressures. This small opening is created in the iris, the colored tissue within the eye. In the distant past iridotomies were accomplished through surgery. Today we are able to create such small openings using a laser, in a clinic setting, which does not require hospitalization. During this laser treatment, called iridotomy, the eye-surgeon creates a small hole through which the pressures in the eye can be equalized by creating an additional pathway for flow between two different compartments within the eye.
It is important to note that this laser treatment is suited only for very specific types of glaucoma, known as closed-angle glaucoma, and narrow angle glaucoma, and that it is not appropriate for (doe not help) other types of glaucoma. Your ophthalmologist is experienced in diagnosing which kind of glaucoma you have, and furthermore, deciding which one out of the tens of possible glaucoma treatments is the right treatment for you. Matching the right treatment to your eye condition is such a specific process that it is not uncommon that the right eye of a certain patient will receive entirely different treatment than the left eye; this is essentially the science and the art of treating glaucoma. Therefore, in cases of uncertainty it is often beneficial to consider consulting another ophthalmologist who specializes in glaucoma in the framework of a second opinion.
Thus, the goal of treatment that is carried out for an acute attack of closed-angle glaucoma is freeing the obstruction and thereby reducing the eye intraocular pressure. However, then the question arises, what will be the fate of the other eye? It turns out, that many research studies have shown that the risk for the second eye also developing such an attack during the patient’s lifetime can be as high as 50% or more. The patient, therefore, is faced with a number of options. One (wrong) option is to wait for the onset of the attack in the second eye and then treat it similarly to how the first eye was treated. Another option is to offer the patient laser treatment (iridotomy) now, with the intention of preventing the future attack from taking place in the second eye. It is hence the right decision for any person who experienced this type of attack to undergo a preventive (prophylactic) laser treatment in the healthy eye, which did not experience yet a devastating acute angle-closure attack.
We will move on now to my next question, a slightly more difficult one: what would you recommend for a person whose ophthalmologist, during a routing exam, diagnosed (unexpectedly) a condition of a narrow-angle, with significant risk for developing an attack at some point in the future? Is it better for that person to come to terms with the risk that at some point in the future an attack might, or will, develop, or perhaps it is preferable to undergo a preventive laser treatment? The answer to this question depends, in my opinion, on the percentage of risk for a future attack. In order to clarify myself I will use the following example: if the risk is estimated at 1%, most people might happily opt out of preventative laser treatment. However, if the risk were estimated at 90%, then any intelligent person would prefer the prophylactic treatment over the high probability of experiencing an acute and dangerous attack whose intensity and danger may be compared to a: “heart-attack of the eye.” If so, the decision whether or not to offer pre-emptive laser treatment for a particular eye is in large part connected to the amount of risk of developing a future attack, and this is dependent largely on the degree of narrowing of the angle and in additional factors that are evaluated when your eye doctor examines your eyes.
Your ophthalmologist is capable of establishing the degree of narrowing of the angle in each of your eyes, and with this information can assess whether the eyes are at any significant risk for developing an acute attack in the future. The glaucoma specialist to whom you may then be referred to will check you thoroughly, as well as specifically for this problem, and will utilize his/her experience and discretion in order to judge whether the risk for an acute attack justifies a preventative laser treatment, called iridotomy, or if the risk is too low to substantiate such treatment at present. If the decision is difficult (as can often be the case) or if the patient is hesitant about agreeing to a laser procedure in an eye that he/she have always felt, up until that point, is perfectly healthy, one can always seek a second opinion. If the degree of narrowing is not critical, the physician can occasionally recommend that the patient consider the option for a few weeks and return for follow-up to continue to weigh the different options. The options just presented are reasonable avenues to help reach the goal of allowing each particular patient to make the decision that is best suited for him/her.